Faced with the threat of a heatwave, a nationwide prevention and action plan has been established in France: Plan Canicule 2022.
Here is a summary of it for families newly arrived in Provence to show how it works; included are instructions on recognizing and coping with heat-related health problems, published by Dr Franck Scola.
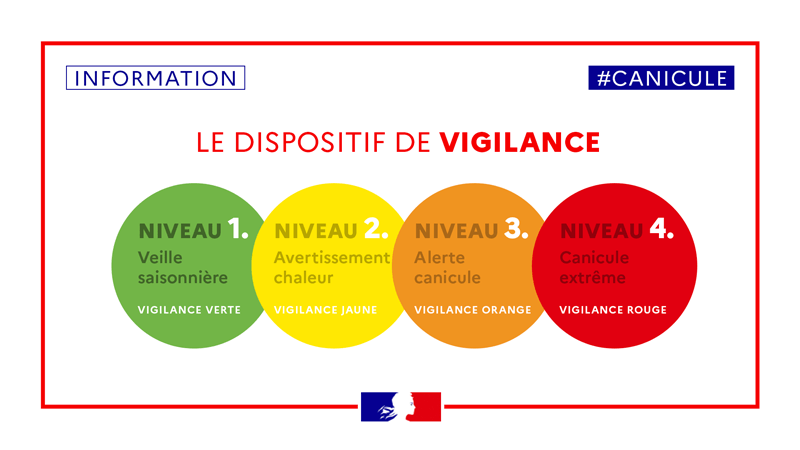
⚠ The Plan Canicule 2022 is organized into four levels according to risk levels:
– The first one is the level of « veille saisonnière » (seasonal surveillance) that has been officially activated by opening a helpline: called “canicule info service”: 0 800 06 66 66 (free from a landline, from Monday to Saturday, 9:00 to 7:00 PM). This first level also corresponds to the installation of the biometeorological monitoring device, provided by Météo-France and the Institut de Veille Sanitaire (INVS), in order to detect the possible occurrence of heatwave.
– The second level of “avertissement chaleur » (Warning and Actions, Heat Warning) is triggered by the prefects of the departments concerned when weather conditions require.
– The third level of « alerte canicule » (Heatwave Warning) is triggered on the instructions of the Prime Minister if the heat is associated with other factors (shortage of drinking water, healthcare system saturation…).
– And the fourth level, of « canicule extrême » (Extreme Heatwave).
This Plan Canicule 2022 is based on five principles:
– Measures to protect people at risk
– Tracking of people at risk, via municipalities’ registers of frail and isolated residents
– Alerts based on the biometeorological evaluation
– Support measures: permanent care and home help services; voluntary associations
– Public information systems for the general public, professionals and health facilities.

👥 Who is at risk?
Although anyone at any time can suffer from heat-related illnesses, some people are at greater risk than others.
Newborn babies, toddlers and children are sensitive to the effects of high temperatures and rely on others to regulate their environments and provide adequate liquids.
The elderly may not compensate for heat stress efficiently and are less likely to feel and respond to changes in temperature.
The overweight may be prone to heat sickness because of their tendency to retain more body heat.
Other categories are particularly vulnerable: pregnant women, people with chronic diseases (renal, cardiac, respiratory, thyroid …), those taking certain types of medication, alcoholics, drug addicts, people doing sport where physical efforts produce heat and water loss, some professionals exposed to heat and /or to insufficient water supply.
🌡Consequences of heat exposure on health:
– We suffer heat-related stress and/or illness when our body is unable to compensate and properly cool itself. Normally it does so through perspiration. Under some conditions, this isn’t enough and in such cases, body temperature rises rapidly.
– A sudden increase of temperature and even short periods of high temperature can lead to serious physical stress, possibly damaging the brain and other organs.
– Heavy perspiration, in addition to water loss, also removes salt and minerals from the body.
– Some situations resulting in the increase of heat production and water loss from the body may include: intense physical activity; prolonged car driving; long exposure to an overheated environment; drinking alcohol, tea or coffee and certain medicines.
– Sunburn affects the body’s ability to cool itself and causes a loss of body fluids. It also damages the skin.

🩺 Examples of heat-related illnesses:
Heat stroke, heat exhaustion, heat cramps, sunburn, heat rash, pyelonephritis, kidney stones, aggravation of a pre-existing disease, infant convulsion…
❗ The main symptoms suggestive of heat-related illnesses:
Fever, Red, hot and dry skin, Thirst, Throbbing headache, Aggressiveness, Dizziness, Nausea or vomiting, Muscle cramps, Tiredness, weakness, Fainting, Concentrated urine (dark, strong-smelling), Constipation, Grumpiness in children …
❓ What to do before medical intervention:
For adults:
- Stop all activity and sit in a shady and cool place
- Remove clothes
- Refresh the body (water spray, wet towel, fan, etc)
- Have a cool shower or bath, and drink cool nonalcoholic beverages (to be avoided in case of unconsciousness or vomiting).
- Call your family doctor, or phone 112 for medical information or intervention
With children:
- Try to be calm and reassuring
- Place the child in an air conditioned room
- Undress the child
- Cool with spray or towel; put their hands under a faucet of running water, their feet in a basin of cold water,
- Let the child rest without going to deep sleep
- Give a dose of Paracetamol (Doliprane® or Efferalgan®) orally if possible, suppository in case of vomiting
- Hydrate and supplement minerals, preferably with hydration solution (GES45®, Adiaril®), very slowly to avoid vomiting. Using a syringe is very handy for persuading young children to drink.
- In all cases, call your family doctor or 112
💡 Prevention:
During hot weather, to protect your health, remember to keep cool, well hydrated, and use your common sense. The following tips may be helpful:
- Drink plenty of fluids
Don’t wait until feeling thirsty. Drink mainly water, at least one glass per hour between meals (more if your activity requires it).
If urine is abundant, transparent and odourless, then you are drinking enough.
Avoid alcohol, tea and coffee as these drinks increase the body temperature and make you urinate more.
Do not drink diuretics unless they have been medically prescribed.
Ensure your children take a drinks break when playing.
For small children, a syringe to drink from is better than a baby bottle to ensure that they swallow.
If your fluid intake is limited by a medical condition, consult your family doctor in hot weather.
- Intake of salt and minerals
To compensate for salt and minerals lost by perspiration, drink sports drinks or a hydration solution.
If you are on a low-salt diet, talk with your doctor before taking sports drinks or salt tablets.
These measures are important only for those with intense physical activities in high temperatures.
Salt and minerals from food are normally sufficient, so avoiding skipping meals is advisable
- Schedule outdoor activity carefully
From about 11 AM to 4 PM, try to stay cool indoors, limit physical activity, car driving and sun exposure.
- Wear appropriate clothes and sunscreen
Wear as little clothing as possible when you are at home. Try to choose lightweight, loose-fitting and light-coloured clothing.
If you must go outdoors, protect yourself from the sun by wearing a wide-brimmed hat, sunglasses, and wearing high-factor sunscreen.
- Avoid hot food, heavy meals and alcoholic drinks; they increase body heat.
- If you are on long-term treatment, ask your doctor if you need to change it. Certain medicines increase body temperature, some eliminate water, and others may be modified by heat.
- Protect those who are at high risk.
For more information, don’t hesitate to phone the special helpline: 0 800 06 66 66
In an emergency, phone 112 if your family doctor is not available.